A rare and aggressive form of breast cancer threatens fertility in many young women. It’s also notoriously hard to treat. Yet, with quick intervention and modern treatment, one survivor beat the odds, stunning even seasoned doctors.
Shelly Battista doesn’t use the phrase “It’s a true miracle” lightly. After enduring aggressive treatment that resulted in the removal of both her breasts and ovaries, doctors told her natural conception was no longer possible. Yet, defying all expectations, she gave birth to identical twins.

Shelly Battista with her husband and oldest daughter at a breast cancer awareness event, dated January 12, 2023 | Source: Facebook/northwesternmedicine
At the center of Shelly’s journey is a rare form of cancer—one with limited treatment options and even fewer certainties. But thanks to groundbreaking medical advances and courageous, life-altering decisions made during her most vulnerable moments, she now shares her home with three children.

A doctor holds Shelly Battista’s newborn twins at the hospital, dated January 12, 2023 | Source: Facebook/northwesternmedicine
Triple-Negative Breast Cancer and Its Impact on Fertility
For women in their thirties, a breast cancer diagnosis often delivers a dual blow: the urgent battle to survive and the quiet, often irreversible loss of fertility.
Triple-negative breast cancer (TNBC) is a rare but particularly aggressive subtype of breast cancer. Though it represents only a small percentage of cases, it poses a heightened threat to younger women. What sets TNBC apart is the absence of three key receptors—estrogen, progesterone, and HER2—that most conventional treatments target to slow or stop tumor growth. Without these receptors, treatment options are limited, and the cancer tends to spread more quickly, often requiring intensive chemotherapy that can severely compromise reproductive health.
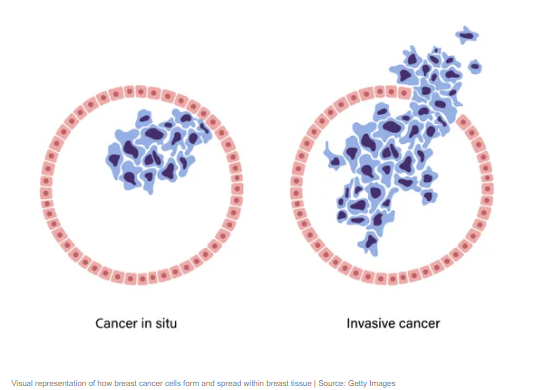
Without those biological entry points, chemotherapy becomes the primary—and often only—effective treatment for TNBC. But while it’s life-saving, chemotherapy is also harsh, particularly for women of reproductive age. It can rapidly damage the ovaries, diminishing hormone levels and depleting egg reserves. For some, this leads to temporary menopause; for others, the loss of fertility is permanent. The effects extend far beyond the physical—stripping away future possibilities before a patient has even had time to fully absorb the reality of her diagnosis.
Adding another layer of complexity, triple-negative breast cancer is often linked to inherited gene mutations—most notably BRCA1 and BRCA2. These genetic mutations don’t just heighten the risk of developing breast cancer; they also significantly increase the likelihood of ovarian cancer.
For patients who test positive, the standard medical recommendation is often preventive surgery to remove the ovaries and fallopian tubes—drastically reducing, if not eliminating, the chance of future pregnancy. Yet amid the urgency and fear, there exists a narrow, high-stakes window—a brief opportunity in which fertility may still be preserved. It’s a race against time, made even more intense by the emotional and physical toll of a life-threatening diagnosis.
If caught early enough—and if the patient is physically able to proceed—doctors can initiate hormone stimulation to retrieve eggs for freezing. In some cases, embryos can also be created using a partner’s sperm or donor sperm. But this entire process must be completed before chemotherapy begins, often requiring action within just days of receiving a diagnosis.
Under normal circumstances, fertility preservation is a carefully timed sequence of steps: daily hormone injections, frequent ultrasounds, blood tests, egg retrieval, and finally, freezing the eggs or embryos. But when layered on top of a cancer diagnosis, that delicate choreography turns into a race—an emotional and medical sprint against the clock.
Delaying chemotherapy increases the risk of the cancer spreading. Forgoing fertility preservation, on the other hand, can mean giving up the possibility of having biological children. Striking a balance between these two paths has become one of the most difficult—and defining—dilemmas in modern oncology.
Shelly confronted that dilemma before she’d even had time to absorb the full weight of her diagnosis. She was 34, still settling into life as a first-time mother, when she was suddenly forced to make an impossible decision: begin the urgent fight for her life, or pause—briefly—to try and preserve the future she had always dreamed of, one that included more children and the family she had imagined for years.
A Missed Signal, a Rushed Decision
Shelly had just begun to settle back into the rhythm of working motherhood when something felt off. It was February 2020, and while pumping at the office, she noticed a lump in her breast. Assuming it was a clogged duct—common among nursing mothers—she brushed it off and carried on.
But the lump didn’t go away. Weeks passed, and with them, the crucial window for early detection began to close. Shelly had no family history of breast cancer, no known genetic predisposition. And as the COVID-19 pandemic upended daily life and delayed routine medical care, her evaluation was pushed further down the line—buying time for the cancer to grow, unchecked.
It wasn’t until May—three months after first discovering the lump—that Shelly received a formal diagnosis: triple-negative breast cancer. She was caring for a six-month-old baby and now facing a particularly aggressive cancer known for its rapid progression and limited treatment options. “We were just starting our life together,” her husband, Robert Battista, later recalled. “And we get this shocking news.”
Within days, genetic testing brought another blow: Shelly carried mutations that significantly increased her risk for ovarian cancer. That discovery reshaped her treatment plan. Chemotherapy was only the beginning. To protect her long-term health, she would also need a double mastectomy and surgery to remove both her ovaries and fallopian tubes—procedures that would permanently end her ability to conceive naturally.

But before any of it could begin, there was one final chance—if it wasn’t already too late. Shelly was referred to Dr. Kara Goldman, a reproductive endocrinologist at Northwestern Medicine. With precious little time to act, she began hormone injections just two days after her diagnosis.
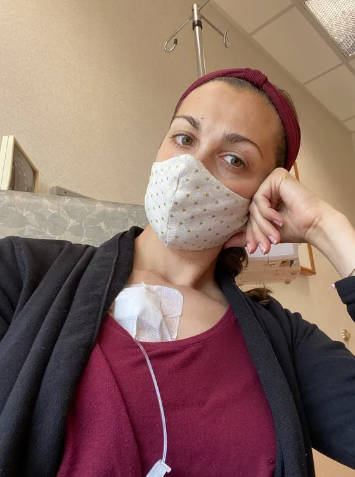
Over the next two weeks, Shelly went through the full course of fertility preservation: daily hormone injections, frequent blood tests, and ultrasounds to stimulate and monitor her ovaries. The process was physically taxing and emotionally overwhelming. She was gearing up for the fight of her life while trying to protect the future that cancer threatened to take away.

At the end of those two intense weeks, doctors successfully retrieved and froze eight embryos. They wouldn’t be needed right away, but they symbolized hope—a choice made just in time, before treatments that would end Shelly’s chance of conceiving naturally.
Chemotherapy, Surgery, and the End of Natural Fertility
Shelly’s treatment began immediately after her fertility preservation cycle. The first phase was 12 rounds of chemotherapy, each designed to halt the cancer’s spread, each one taking a toll on her body and pulling her further away from the life she had just welcomed months before.

As the weeks passed, Shelly prepared for the next phase: surgery. A double mastectomy was the standard recommendation for patients with triple-negative breast cancer, especially those carrying BRCA gene mutations. Without hesitation, Shelly chose to proceed—the priority was clear: survival above all else.
Yet the emotional weight of what she was losing—her breasts, her strength, and soon, her chance at natural motherhood—never left her side. While the cancer responded to treatment, her doctors remained deeply concerned about her heightened genetic risk for ovarian cancer.

To safeguard her long-term health, doctors recommended a bilateral salpingo-oophorectomy—the surgical removal of both ovaries and fallopian tubes. By the time Shelly finished her treatment, the organs necessary for natural conception were gone.
Her uterus remained intact, but the ovaries that had once been stimulated to produce the embryos she’d frozen just weeks earlier were no longer there. Still, she had done everything possible to preserve hope. The embryos were safely stored, and Shelly was now cancer-free.

Rebuilding Possibility: Pregnancy Without Ovaries
One year after finishing treatment, Shelly was ready to take the next step. “The ovaries and the uterus function very independently of each other,” explained Dr. Kara Goldman, Shelly’s fertility specialist at Northwestern Medicine. In cases like Shelly’s, hormone replacement therapy can prepare the uterus to support a pregnancy.
“Because she no longer had ovaries producing hormones,” Dr. Goldman added, “we were able to provide her with the necessary hormones to make pregnancy possible.”
The first two embryo transfers didn’t succeed. Each failure brought disappointment, but never defeat. Then, on the third attempt, Shelly got a call directly from Dr. Goldman—the embryo had implanted. She was pregnant. “We were both ecstatic—crying and yelling,” Shelly recalled.
For Robert, the news was more than just a relief. “It was just awesome. We were going to have another kid, Shelly was healthy, and it felt like everything was behind us,” he said. But what came next was something neither of them had expected.

A Rare Twin Pregnancy and the Day Everything Came Full Circle
After the successful embryo transfer, Shelly went in for a routine ultrasound. The transfer had involved just one embryo—carefully chosen from the eight frozen before her chemotherapy. But the scan revealed something surprising: she was expecting identical twins.

The embryo had split after implantation—a rare occurrence happening in about 1 percent of cases, according to Dr. Goldman. There was no medical intervention or fertility technique intended to increase the chances of multiples; it simply happened naturally.
Despite Shelly’s complex medical history, her pregnancy progressed smoothly. Her uterus responded well to the carefully managed hormone support, with no complications or setbacks. All that remained was the wait and the countdown to delivery. Shelly was scheduled for induction at Northwestern Medicine Prentice Women’s Hospital

Shelly Battista’s daughter, Emelia, stands beside her newborn twin sisters, dated January 12, 2023 | Source: Facebook/northwesternmedicine
The date chosen was December 9, 2022—exactly two years after Shelly completed treatment and was declared cancer-free. This coincidence wasn’t planned by her medical team, but for Shelly and Robert, it gave profound personal meaning to an important clinical milestone. Their daughters, Nina and Margot, were born that day.
“Despite a breast cancer diagnosis, chemotherapy, and losing both ovaries, Shelly’s dream of having three children came true,” Dr. Goldman later reflected. “One perfect embryo, frozen urgently before chemotherapy, became two beautiful baby girls.”

Shelly Battista’s newborn twins sleeping side by side, dated January 12, 2023 | Source: Facebook/northwesternmedicine
“It’s a true miracle,” Shelly said. “We have two babies, exactly two years cancer-free. My heart is very full.”
Months after the twins’ birth, Shelly appeared on the Today Show, sharing her reflections on life after cancer and motherhood—a powerful testament to hope, resilience, and the unexpected joys that can emerge from the darkest moments.

“Lots of laughs, lots of cries, and lots of laundry,” Shelly described her daily life. “It’s chaotic, but it’s perfect.”
At that time, she and Robert were adjusting to life with three children—Emelia, Nina, and Margot. Their family’s incredible journey resonated widely, sparking an outpouring of support and emotion online.
On Instagram, the comments flooded in. “Congrats! What a beautiful story. You are a strong mama,” one user wrote, capturing the heartfelt response from thousands touched by Shelly’s story.

Another user wrote, “Congratulations… what a blessing,” while someone else reacted with a simple, “Awesome!!!”
Another added, “What a wonderful story!!” One commenter called Shelly a “warrior mama” and echoed, “Congratulations!”
The outpouring of love and encouragement was a testament to the power of hope and resilience in the face of adversity.

